Navigating Complexity: Understanding and Addressing Challenges Faced by Kurdish Women with FGM/C

By Osman Mahmoudi UNICEF reports that FGM/C remains prevalent in Iraqi Kurdistan, affecting over half of women who live there. The profound impact of this practice requires urgent medical and psychological support for survivors. However, a lack of specialized professionals in the region, and limited awareness of treatment options and complications, pose challenges. Cultural taboos and social constraints further impede survivors from seeking help, leading to discrimination, stigma, and reluctance to access essential services. As a family counselor and psychotherapist specializing in FGM/C, I have conducted extensive research and provided psychological, sexual, and physical services to survivors and their partners. Between 2019 and 2023, I conducted numerous workshops for local teams in Iraqi Kurdistan, focusing on effective communication with survivors and providing comprehensive care. These sessions focused on understanding the complications of FGM/C and breaking the taboo’s surrounding the discussion of this practice. The workshops highlighted the lack of readily available psychological support for survivors, as well as cultural and social obstacles they face in opening up about their struggles. They also highlight how professionals – like doctors – lack awareness regarding proper treatment methods for FGM/C. However, participants’ eagerness to learn and enhance care emphasized the need for continuous education and training in this domain. These experiences underscore the potential for improving survivor care through ongoing learning and educational initiatives. In 2023, after concluding the training sessions, the educational materials used were compiled into a publication titled “Living with FGM in Kurdish Regions.” This book aims to fill a significant gap in existing literature, and serves as a guide to help survivors enhance their quality of life. The book comprises five chapters, each of which explores various aspects of FGM/C: The first chapter dives into the historical and cultural context of the practice in Iraqi Kurdistan Chapter two focuses on the challenges Kurdish women face in openly discussing their experiences Chapter three stresses the importance of addressing survivors’ physical health through comprehensive medical examinations and management strategies Chapters four and five explores the psychological and sexual impacts of FGM, offering insights into therapeutic interventions As a handbook, this publication also provides practical guidance on psychosexual therapy and social services. It marks a culture-oriented approach in the domain of “Life with female circumcision,” emphasizing the importance of respecting and empowering survivors while tailoring therapeutic approaches to their individual needs. Osman Mahmoudi is a family counseling doctor, researcher, and trainer specializing in FGM in Iran. His research aims to enhance the psychosexual well-being of FGM survivors by improving access to quality healthcare in the region. He earned his doctorate in family counseling from Shahid Chamran University of Ahvaz. Additionally, Osman Mahmoudi is dedicated to advancing sexual rehabilitation for FGM survivors in Kurdistan, Iran, through his ongoing study. Related links: This Father’s Day, join our campaign Survivor Support Resources
Training the Prince George’s County Health Department on FGC
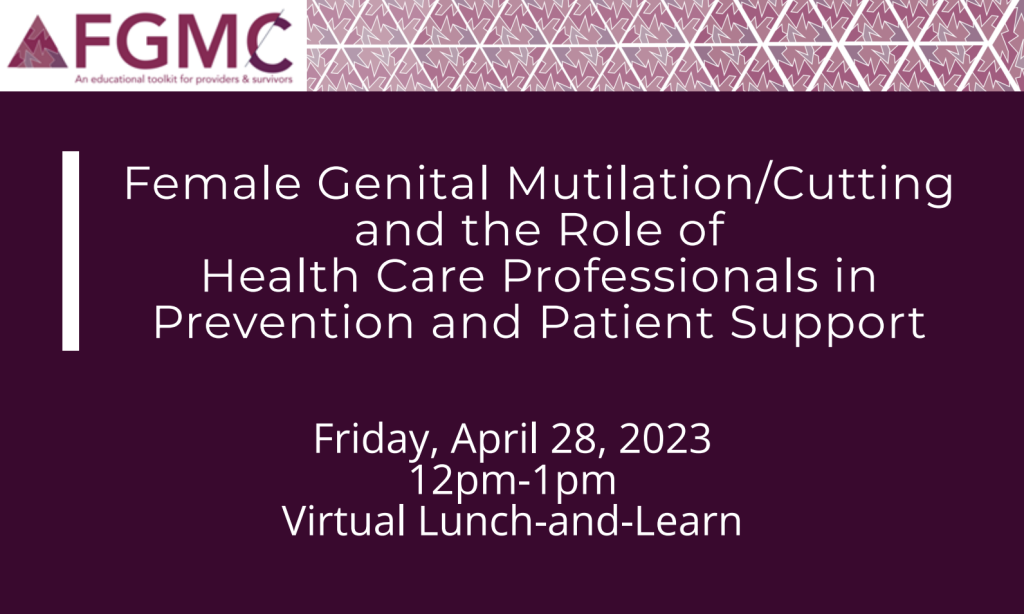
On April 28th, Karen McDonnell, Associate Professor at George Washington University’s Milken Institute School of Public Health partnered with Sahiyo Cofounder Mariya Taher to provide a training for nearly 70 health care providers at the Prince George County Health Department on female genital cutting (FGC) and the role of health care professionals in prevention and patient support. Health care providers are important first-responders when it comes to servicing those impacted by FGC, and there is an ever demanding need for culturally cognizant and sensitive training for health care providers in the U.S. This training provided information on the impact of FGC in the U.S. along with practical guidance on how to work with survivors. Resources such as GWU’s Educational FGM/C toolkits for providers were also shared.
Exploring Canadian physicians’ experiences providing FGC-related care

By Kiah Leone As countries like the United States, Canada, Australia, and others become increasingly aware of the practice of female genital cutting (FGC) and its presence in their country, their healthcare systems are having to explore what support and quality services for survivors of FGC entail. Medical studies conducted across many of these countries have identified a significant lack of knowledge on behalf of healthcare workers when it comes to the practice of FGC. This lack of understanding regarding the practice, particularly the various sociocultural contexts within which it is perpetuated, can often leave survivors confronted with a healthcare system ill equipped to meet their particular needs. Unfortunately, instances of discrimination and stigmatization are not uncommon as a result, and such instances may cause survivors to feel discomfort, judgement, embarrassment, and fear in medical contexts, or to avoid seeking medical help and attention altogether. As part of my graduate degree in Social Anthropology, I decided to investigate the experiences of medical professionals in Canada as they navigated appropriate and culturally competent care for survivors. In 2018, I conducted a qualitative study with interviews of Canadian physicians and health care providers who had provided reproductive health care to survivors in Canada. The purpose of this study was not only to gain a deeper understanding of the role of physicians and medical personnel in providing reproductive health care to survivors of FGC, but to also learn how FGC was thought about, both within the Canadian healthcare system and in Canada as a whole. Interviews with medical professionals consisted of a series of questions regarding their level of education and training, experiences providing reproductive health care, knowledge of FGC and how they first came to learn about it, as well as their experiences providing care specifically for survivors. From these interviews, four major themes emerged: a lack of education and training amongst health care personnel in regards to FGC; reliance upon repeated encounters with survivors in order to develop a form of expertise in FGC-related care; a desire amongst participants to educate past, present, and future health care professionals on the practice of FGC; and the belief that FGC is an important topic of concern for reproductive health care specialists in Canada. What stood out across each of these themes was an emphasis on the importance of understanding FGC, rather than just learning how to accommodate survivors within a medical context. The physicians and health care providers who participated in my study all recognized the value and importance of education, training, and mentorship in the medical and health care concerning FGC in Canada. Providers explored the benefits of education and training, not only for their current and future medical students and residents, but also for their colleagues and peers to account for the diverse needs of their patients. From this study, I concluded that by continuing their own learning, making recommendations, and implementing education initiatives that provide early learning opportunities for others, Canadian health care professionals can improve the quality of care that survivors receive here in Canada. Kiah Leone (she/her) is a Doctoral Candidate in the School of Health Sciences and an Instructor for the Department of Anthropology at the University of Northern British Columbia (UNBC). Kiah’s research interests focus on improving female genital cutting (FGC) survivors’ experiences in accessing quality health care in Canada. She received her MA in Social Anthropology from York University and her BA in Anthropology from Vancouver Island University. Kiah is currently undertaking a study on the introduction of clitoral reconstructive surgery in Canada.
Female Genital Mutilation/Cutting (FGM/C): A survey of knowledge, attitudes, and practices of health care professionals in urban/ rural India

Female genital mutilation/cutting (FGM/C) has been performed on an estimated 200 million women and girls worldwide. Health care professionals play a significant role in the prevention of FGM/C. They can support and educate patients and communities about the advantages of ending the practice. However, health care professionals (HCPs) frequently lack the resources and education required to carry out these crucial duties. Until February 28th, 2023, a team of researchers from India is conducting a survey among health care professionals regarding their knowledge, attitudes, and practices (KAP) about FGM/C. Who is this survey for? Doctors (MBBS or postgraduate including AYUSH), nurses, and midwives practicing in urban/rural India. Our goals for this survey: to assess the KAP of health care providers; to establish a baseline for further research in India; to help facilitate the creation of efficient plans, policies, and targeted training initiatives on how to deal with FGM survivors (medically and psychologically) in the future for HCPs; to create awareness among health care workers in India. Any health care professional who is eligible according to the criteria can provide their insights about FGM/C by filling out this survey. It consists of roughly 30 questions which should take approximately 5 minutes to complete. Who can you reach out to? If you have any queries, feel free to contact the researchers at: alifya104@gmail.com or saadkazi5484@gmail.com.
