Reflecting on the ‘How to Stop The Rising Trend of Medicalising Female Genital Cutting in Asia’ webinar

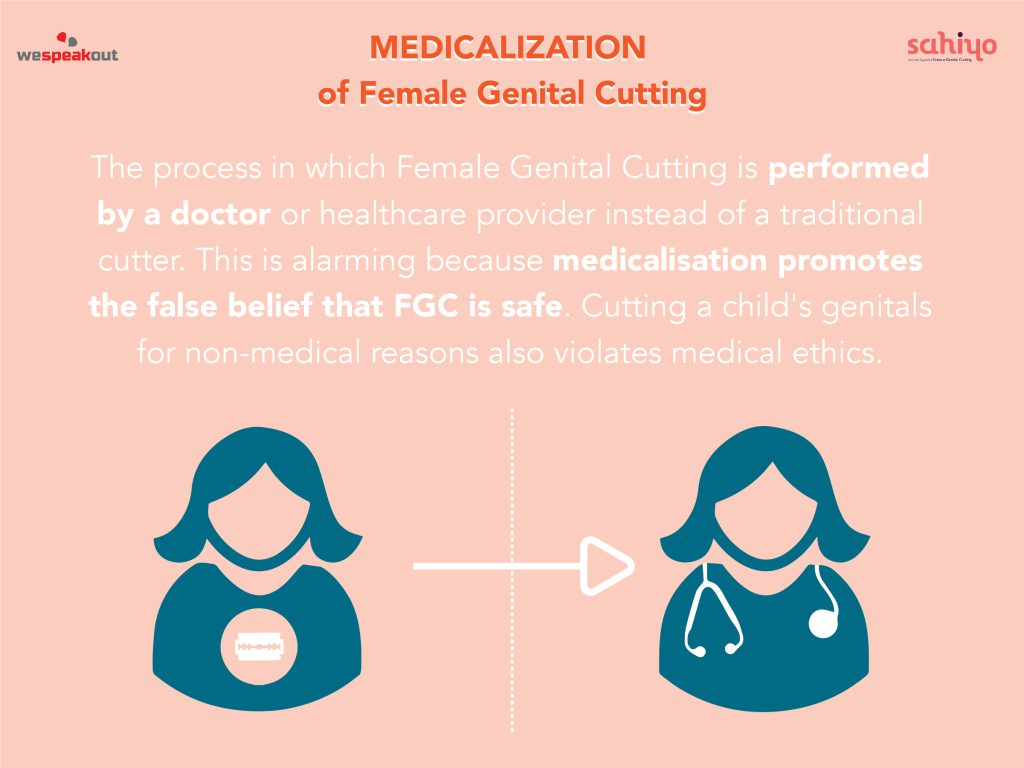
On January 20th, Sahiyo hosted the webinar ‘How to Stop The Rising Trend of Medicalising Female Genital Cutting in Asia’. Organised by Sahiyo’s program’s intern Beth Fotheringham and moderated by Sahiyo co-founder, Insia Dariwala, the webinar featured a panel of experts in female sexual and reproductive health: Saza Faradilla, Kalpana Swaminathan, Ibu Atas, and Dr. Nozer Sheriar. The discussion was centred around two main questions: Why does the medicalisation of female genital cutting need to be stopped and how can we stop this rising trend? Sahiyo Intern Beth began the event by providing a brief overview of female genital cutting (FGC), citing motivating factors for the practice such as social acceptance, marriageability, community belonging, proof of virginity, curbing promiscuity, hygiene, and religion. Though there are no health benefits to medicalised FGC, there is often a misguided belief that the procedure is safer when medicalised. The medicalisation of FGC refers to situations in which FGC is practised by a healthcare professional, whether in a public or a private clinic, at home or elsewhere. More than 200 million women and girls have experienced some form of FGC, with 1 in 3 girls being cut by a health professional. The following video shared during the webinar highlights that many young girls undergo this practice against their will. [youtube url=”https://www.youtube.com/watch?v=k6zpXf6Gm4k”] By courageously sharing her voice and her story, Saza Faradilla gives us an insight into how the practice is carried out without consent. Her story showcases the trauma experienced by survivors who only discover that they have suffered FGC as an adult. This speaks to the aura of silence that surrounds the practice. A lack of questioning falsely leads people to believe that FGC is necessary for socio-cultural or religious reasons. In Singapore 20.5% of doctors carry out FGC, 9.4% of which perform FGC on girls before their first birthday. The preferred age for cutting is between 4-6 months. The backlash Saza receives in her community highlights the need for change. By speaking out against what is perceived to be normal in her community, she recognises that her right to health, the right to physical integrity, and the right to equality and non-discrimination have been violated. Saza’s heartfelt and inspiring activism demonstrates that human rights emerge and evolve through the attempts of ordinary people to challenge injustice. Saza embodies the power of storytelling by sharing stories; hearing a survivor’s experience can definitely shift attitudes and opinions on this issue. The significant lack of information surrounding FGC and medicalization is driving the practice. This means that individuals, including doctors, conform to the norm of FGC without being aware of its inequalities. Pressure to conform to social expectations is a motive behind why healthcare professionals perform FGC. Carrying out FGC in hospital or health settings creates a false sense that FGC is necessary. FGC does not take the bodily integrity of the child into consideration and there is a misogynistic link to FGC being medicalised. Portraying that cutting can be done ‘cleanly, neatly and safely’ directly translates into control of female sexuality and results in the subordination of women. Kalpana expressed how FGC injures much more than the child’s anatomy – any child that suffers unwanted touch will deal with a myriad of mental and psychological effects. However, Kalpana notes that this trauma can also translate into a determination in survivors to fight back and speak out against the wrong-doing they have suffered. Kalpana Swaminathan further develops the argument against the medicalisation of FGC, stating that there is no room for the medicalisation of FGC and the practice cannot be condoned. She explains how the power of culture and tradition can make individuals think and act collectively. Therefore, changing the attitudes of parents and doctors is integral in the campaign to eradicate FGC. How can we stop this rising trend? FGC is not only happening in Asian communities, it is happening everywhere in the world. Sahiyo co-founder Insia Dariwala raised pressing questions such as how do we hold doctors responsible and who is going to do it? Ibu Atas, long standing activist for FGC in Indonesia explains that a firm stance is needed in the work against this practice. FGC is deeply embedded in culture. By campaigning against this practice, we are challenging community attitudes, social norms and their values. Taking immediate action is the best response to the rising trend of medicalising FGC. The message I took away from this webinar ties in with Sahiyo’s objective to recognise and emphasise the values of consent, as well as a child and woman’s right over her own body. Our speakers stressed that there are no justifications for FGC, regardless of who carries it out. Kalpana explains that parental attitudes are influenced by social norms and refers to consent as ‘a can of worms.’ This made me realise that understanding how parental attitudes influence the practice of FGC is key to developing appropriate interventions aimed at eradicating this practice. As put by Ibu Atas, the message must be clear: ‘Don’t touch our genitals.’ Every female should have the right to make autonomous decisions about her own body and reproductive functions. This right is at the core of her basic human rights. Sahiyo would like to thank our panelists for bringing their thought-provoking perspectives to this discussion. You can learn more about the esteemed speakers here. Watch the full event here: [youtube url=”https://www.youtube.com/watch?v=Tqw9OCLmzzU”]
Introducing the Speakers for ‘How to Stop the Rising Trend of Medicalising Female Genital Cutting in Asia’

On January 20th at 4:30 IST, Sahiyo will host a webinar titled ‘How to Stop The Rising Trend of Medicalisation of Female Genital Cutting in Asia,’ which will feature a panel discussion with medical experts and gender rights activists who specialise in sexual and reproductive health. The medicalisation of female genital cutting (FGC) is an increasing issue in a number of Asian countries; a stark lack of legislation concerning the practice has contributed to a medical normalisation of FGC. Our panelists will explore medical perspectives about medicalisation and the current ethical debate surrounding this phenomenon, and touch upon the safety concerns and question of consent that underpins much of the controversy. We will be joined by Sahiyo co-founder Insia Dariwala, as well as Saza Faradilla, Ibu Atas, Ajali Nayyar, Dr. Kalpana Swaminathan, and Dr. Nozer Sheriar. If you’re interested in joining our webinar, please see more information and sign up here. About our Speakers: Saza Faradilla: Saza is a co-founder of End Female Genital Cutting Singapore (End FGC SG) whose vision is a Singapore where FGC is obsolete. Some of their activities include organising panels on the social, religious and medical aspects of FGC, support sessions for survivors of FGC, and lobbying political, religious and community leaders to release public statements on FGC. Slowly, but surely, they have managed to broaden the conversation on FGC to include discussions on bodily autonomy, child rights, and consent. Ajali Nayyar: Anjali Nayyar has more than 20 years of experience in global health issues. Her expertise lies in developing integrated strategies to impact health policy and practice in the Global South. She oversees the organization’s programs in emerging markets in Asia and Africa, working through four offices and a network of independent consultants. Prior to joining GHS, she served as Country Director for the Program for Appropriate Technology on Health (PATH) in India. Preceding PATH, she worked with the International AIDS Vaccine Initiative (IAVI) for six years, where she served initially as India Country Director and then as Vice President for Country and Regional Programs in New York. As Vice President, she led field operations and non-research programs in India, Brazil, South Africa, China, Kenya, Rwanda, and Uganda. She is a member of the Confederation of Indian Industry’s (CII) National Committee on Public Health, the Expert Group on Tuberculosis set up by a Forum called Global Coalition Against TB, and the Advisory Group Uniting to End Neglected Tropical Diseases, a WHO mandated organization. Dr. Kalpana Swaminathan: Dr. Kalpana Swaminathan is a Paediatric surgeon and women’s rights activist. She has worked with traumatized children and is concerned with a child’s rights over their body. She also writes along with Ishrat Syed as ‘Kalpish Ratna’, exploring the interface between science and the humanities, and has released a number of books.They are presently working on a history of misogyny. Ibu Atas/Atashendartini Habsjah: Atashendartini Habsjah, affectionately and respectfully known as Ibu Atas, is an inspiring women’s rights activist and independent researcher in sexual and reproductive health and rights. She has been working to end FGM/C in Indonesia since 1994, when, as a lecturer of Women’s Studies at the University of Indonesia, she supported country-level work that influenced the landmark Beijing Declaration and Platform for Action. She began collecting data in the mid-90’s with the authorization of the Indonesia Population Council, starting with West Sumatra and West Java. For the last 10 years, she has been working closely with the Ministry of Women’s Empowerment, the Ministry of Religious Affairs, and the Ministry of Health to stop FGM/C in Indonesia, and in particular, the high medicalization of the practice, in close collaboration mid-wives, nurses, and gynecologists. She hopes that FGM will disappear in Indonesia during this generation and before 2030. Dr. Nozer Sheriar: Dr. Nozer Sheriar is an obstetrician and gynecologist with a longstanding commitment to advocacy for and the promotion of women’s rights and access to safe abortion. He practices at the Breach Candy, Hinduja Healthcare Surgical and Holy Family hospitals in Mumbai. He currently is a member of the Governing Boards of Ipas, the Guttmacher Institute and Centre for Catalysing Change, as well as the Co-Chair of the Medical Advisory Panel, FPA India. He also serves as a member of the Technical Advisory Group on Maternal and Child Health and the Technical Sub Committee for Sexual Reproductive Health of the South East Asia Region of the WHO. As Past Chairperson of the MTP Committee, FOGSI and member of the Technical Advisory Panel, Ministry of Health and Family Welfare, Dr. Nozer participated in the amendment of the MTP Act, the development of the national comprehensive abortion care guidelines, and conducted multicentric research. In acknowledgement of his dedication to and support of women’s healthcare he has been awarded the FRCOG Honoris Causa by the RCOG.
Sahiyo India to host a panel discussion on ‘How to Stop the Rising Trend of Medicalising Female Genital Cutting in Asia’

On January 20th at 4:30 IST, Sahiyo will host a webinar titled ‘How to Stop The Rising Trend of Medicalisation of Female Genital Cutting in Asia,’ featuring a panel discussion with medical experts and gender rights activists from India and Singapore who specialise in sexual and reproductive health. The medicalisation of female genital cutting (FGC) is an increasing issue in a number of Asian countries; a stark lack of legislation concerning the practice has contributed to a medical normalisation of FGC. Our panelists will explore medical perspectives about medicalisation and the current ethical debate surrounding this phenomenon, as well as touching upon the safety concerns and question of consent that underpins much of the controversy. Sahiyo is unwaveringly opposed to medical professionals performing FGC, as we believe it sets an alarming precedent of normalising the practice; we are keen to stress that there are no safe ways to cut a girl’s genitals, and therefore medicalisation is an important issue to address in the work against FGC. During this webinar, we will bring a diverse variety of voices to the panel to discuss the different elements of medicalising FGC, offering their own expert reasons for, and the dangers of, this increasing medicalisation. Our goal is to create a platform to explore the complexities of the shift towards the medicalisation of FGC across the world and to dispel the myth that it is a harmless way to perform the practice. In line with Sahiyo’s mission for women and girls to have autonomy over their body, standing firmly against the medicalization of FGC re-affirms a woman’s right to have control over her body and live her life free of harm. If you’re interested in joining our webinar, please see more information and sign up here.
A reflection on the medical perspectives on female genital cutting (FGC) webinar

By: Amela Tokić On October 9th, 2021, community-led movement End FGC Singapore, which strives to empower Muslim communities in Singapore to end the practice of female genital cutting (FGC), hosted a virtual event to bring more attention to the medical impact and medicalization of FGC. Saza Faradilla, co-founder of End FGC Singapore and facilitator of the event, introduced the historical background of FGC in Singapore and the rise of FGC medicalization. Guest speaker Dr. Ida Ismail-Pratt shared her medical perspective on the sexual, physical, and psychosocial impacts of medicalized FGC on women and girls. While the full event will not be published, End FGC Singapore will be sharing snippets on its Instagram page. The Medical Perspectives on Female Genital Cutting (FGC) webinar dove deep into the impact FGC poses through migration, with a particular focus at western countries as well. This gave an interesting perception of FGC as a deeply rooted cultural norm, and thus many women and girls born in western countries would seek out FGC in the countries they had migrated to; alternatively, they could be forcibly brought back to their origin countries for the procedure, if FGC is not legally accessible in the migrated countries. This left many participants pondering and asking the questions: Is there a medically safe way to perform FGC? How would I recognize if FGC was performed on me? Is there a difference in consequences when FGC is performed on adults or infancy? My personal highlight from the event was hearing Dr. Ida Ismail-Pratt share professional studies on the sexual impact FGC has on women. The studies focused on both women who have not undergone FGC and those who have undergone FGC, and it concludes that sexual desire is not impacted by having undergone FGC or not. This is a powerful statement, as many who undergo FGC are believed to have a lessened sexual drive as a result. However, the primary impact FGC has on women is the effect it poses on their sexual experience(s) – lower sexual satisfaction. This webinar was a perfect blend of a medical perspective along with a statistical analysis. It not only provided a professional opinion of the impact FGC has on women and girls, but it also provided solid evidence from survivors of FGC as well. One of the most startling findings is that the majority of women and girls are not even aware that they have undergone FGC, since it was done at such an early age. If they are aware, they often do not know who performed the procedure or with what medical instrument. For those interested in being part of future virtual events hosted by End FGC Singapore, you can follow them on Instagram and/or Eventbrite. Read more about past webinars and/or donate to support the end of FGC in Singapore.
Mutilation or enhancement: A researcher’s argument for respectful terminology on genital cutting

By Brian D. Earp I have published several papers on the ethics of medically unnecessary genital cutting practices affecting children of all sexes and genders. When my writing touches on the sub-set of these practices that affect persons with characteristically female sex-typed genitals, I have received some pushback for using the term female genital cutting (FGC) rather than female genital mutilation (FGM). An instance of such pushback came from a respected colleague in response to a paper of mine in Archives of Sexual Behavior, in which I argue against the use of ‘mutilation’ in certain contexts, as there is evidence that such stigmatizing language may have adverse effects on the very people who are meant to be helped. Given that this terminological issue is likely to keep coming up, I thought I would share parts of the reply I wrote to my colleague. I hope it can shed some light on at least one plausible way of thinking about such matters. My colleague argued that my use of ‘FGC’ rather than ‘FGM’ is disrespectful because it goes against the recommendation of the 2005 Bamako Declaration adopted by the Inter-African Committee (IAC) on Traditional Practices Affecting the Health of Women and Children. ——— On the matter of disrespect. I have had many conversations with women who consider themselves circumcised, rather than mutilated, and even if they agree that medically unnecessary genital cutting should not be performed on persons who are incapable of consenting, primarily children, they insist that it is harmful, stigmatizing, and paternalistic for others to simply define their own modified genitals as mutilated (a term that implies disfigurement or even an intent to cause harm). They explain that their loving parents, however misguided, did not intend to cause them net harm, just as, for example, Jewish parents who authorize that their sons be circumcised do not intend to harm them, but rather, take an action that is sincerely believed to appropriately integrate the child into an ancestral community. They recognize that, in their own communities, both male and female genital cutting practices are widely seen as improving the genitalia, including aesthetically, which is contrary to the very notion of mutilation. I may not agree with that interpretation myself, but it is not my position to tell these women (or their brothers) that their altered genitals are ugly or disfigured rather than, as they see it, aesthetically (or in some cases, culturally or religiously) improved. I will ask: Were these leaders democratically elected to express the considered opinions of their constituents, or were these leaders self-appointed? At the very least, they cannot have been authorized to speak on behalf of countless Southeast Asian or Middle Eastern women who have been affected by ritual forms of female genital cutting. In any event, I face a choice. I can disagree with the conclusion of these African leaders who seem to feel qualified to speak on behalf of millions of other women, including non-African women, and impose an entirely negative and stigmatizing interpretation of all of their altered genitalia regardless of how those women see their own bodies. Or I can show respect to those women who have shared their stories with me, as well as all the women in various reports and testimonies who have expressed strong objections to the term ‘mutilation’ being forced on them, and who would simply like to have the room to be able to evaluate and describe their own genitals as they see fit. One woman explained her feelings: “In my opinion, the word ‘mutilation’ used in reference to [what happened to me] is a degrading and disempowering term that strips women of their dignity and self-worth. Basically, it is a label that has the power to negatively influence one’s self-identity. If you understand labelling theory you will understand how damaging/influential a term or classification can be to an individual.” She continued with her experience: “Having just about survived my ordeal of forced body alteration I was very aware of the violation to my body. However, the introduction of the term ‘mutilation’ into my consciousness affected me mentally and physically. It made me view myself as an ugly, mutilated, and frowned-upon member of society. There started my journey of self-hate, which presented itself in many forms, including bulimia and social anxiety, to name but a few. To be called the ‘mutilated’ girl by health professionals stripped me of any dignity and covered me in shame on numerous occasions. Thankfully, I no longer see myself as a victim or survivor of ‘FGM’ – I refuse to allow that term to take away my power or to define who I am.” Faced with the choice between respectfully disagreeing with the analysis and conclusion of a group of leaders whose qualification to speak on behalf of others I do not know, versus showing respect to those women, such as the one quoted above, who have asked for the right to determine their own victim status (including whether they regard their genitals as mutilated or otherwise), I choose the latter. Referring to “the event” and “the torture” is using singular language to refer to a plurality of quite different events carried out in different ways by different groups for different reasons. As you know, the World Health Organization (WHO) uses the term FGM to refer to a dozen or more practices, ranging from nicking of the clitoral hood, which does not remove tissue. In many communities, for example in Malaysia, it’s often done by a doctor with sterile equipment and pain control, through to excision of the external clitoris with a rusty implement and no pain control followed by infibulation, as occurs in some rural parts of Northeast Africa, for example. It is entirely accurate to say that all of those quite different interventions are medically unnecessary acts of genital cutting; and I argue that all of them are morally impermissible if carried out on a non-consenting person. I have written about labiaplasty, a common procedure in Western countries. I
Population Council hosts webinar to discuss ending female genital cutting

By Hunter Kessous The Population Council hosted a fascinating webinar, Using Research to Understand and Accelerate The Abandonment of Female Genital Mutilation/Cutting (FGM/C). It was the second of two webinars from a series titled, Evidence to End FGM/C: Research to Help Girls and Women Thrive. The most recent webinar reported some of the findings of a research consortium that began in 2015 and culminated this year. The research spanned eight countries and concluded with how initiatives to end FGM/C may be optimized. Speakers included Bettina Shell-Duncan, University of Washington (moderator); Nada Wahba, Population Council, Egypt; Dennis Matanda, Population Council, Kenya; P. Stanley Yoder, medical anthropologist; and Nafissatou J. Diop, UNFPA. Dr. Matanda spoke on the use of data to inform programming. His research spanned Kenya, Nigeria, and Senegal, and sought to map hotspots for FGM/C. The data pinpointed the areas of each country in which FGM/C is most prevalent. Dr. Matanda’s findings also reveal how factors relating to a girl’s mother influence the likelihood that she will be cut. The results varied by region, but some of these factors included the mother’s ethnic group, her beliefs surrounding FGM/C, and if she herself was cut. The most important takeaway from Dr. Matanda’s research is that considering only national data masks local variations. He recommends linking regional data to subnational policies and efforts to prevent FGM/C from occuring to future generations of girls. Medical anthropologist Dr. Yoder responded to Dr. Matanda’s research, remarking that Kenya was the only country of the three where the level of education of the mother was found to have an effect on the risk of a girl being cut. He proposes modernization, the shift from traditional and rural to secular and urban, as an explanation for Dr. Matanda’s findings. I believe that Dr. Yoder’s theory illuminates a need for ongoing research on this subject that correlates the changes in Kenya’s social, economic, and political growth to changes in the continuation of FGM/C. Following Dr. Yoder’s analysis, Wahba presented her research on the intersection of FGM/C and gender in Egypt. Hers was a qualitative study with multiple intriguing findings. One discovery that I found especially important was that conflicted mothers have been turning to doctors to decide on their behalf whether or not their daughter should be cut. This could be a result of the increasing medicalization of FGM/C in Egypt. Another interesting finding was that if either one of the parents, whether it be the mother or the father, does not want their daughter to be cut, then she will not undergo FGM/C. While many programs working to end FGM/C target the mother as the decision maker, Wahba’s research clearly shows that mothers are not the only influential group. For this reason, more anti-FGM/C programs should shift their efforts to also educate fathers and doctors, particularly in regions with high rates of medicalization. Diop followed Wahba’s presentation to provide analysis of the research. Diop feels strongly that FGM/C is rooted in gender inequalities, yet not nearly enough programs acknowledge this fact. She claims many programs that address cutting are gender blind, focusing too much on the consequences of FGM/C in their approach rather than the root causes for why FGM/C continues in the first place. Diop’s comments were a strong call to action for all advocates to take a gender transformative approach in order to achieve abandonment of FGM/C. More information about this research project can be found here. The webinar can be viewed here.
Part II–Medicalising khatna within the Bohra community: A Struggle of Tradition and Modernity

By Fatema Kakal (This is Part II in a series about female genital cutting within the Bohra community. Read Part I here.) While religion and religious leaders, along with culture and tradition can be drivers of female genital mutilation/cutting (FGM/C), law can play an additional critical role in disincentivizing khatna. The arrests in the U.S. and Australia due to the medicalisation of FGM/C, led to the reiteration of laws in countries that prohibited FGM/C. Laws in many countries around the world critique FGM/C as a human rights violation and child abuse. While some consider these laws to be racist, this leads to a feeling of marginalization and alienation due to the attack on traditional and cultural value systems. People became more conscious of the laws, and began reconsidering khatna, because of the risks involved. These laws helped initiate dialogue and discourse. The Bohras are a fairly progressive and modern community, where traditions are not separate from their modernity, but play a crucial role in consolidating their Bohra identity. Continuing khatna defies Western notions of modernity and embraces tradition. Instead of abandoning tradition, the Bohras are renegotiating the traditional practice and embrace modernity through medicalising khatna. Medicalisation is a tool to modernize and legitimize khatna, but also serves as a technique for social control. By supporting medicalisation, validated by modernity, and establishing khatna as a safe and religious practice, the clergy is reinventing and perpetuating khatna as a traditional practice, responding to external pressures that threatened to marginalize or alienate the Bohras. The clergy is thus reiterating and reinforcing Bohra identity as being one of modernity and tradition. Thus, khatna was no longer taboo, and a growing discourse has led to people taking increasingly different positions, and making more conscious decisions about continuing the practice. While mothers and women of the family used to be primary decision-makers of continuing khatna for the daughters of the family, fathers are increasingly involved in making the decision. It is no longer an extremely hidden practice, and parents do research before making the decision whether or not to cut their daughters. While some people follow mandates by religious leaders, others find it important to follow the law. People are conscious of the potential harm. For the devout, tradition must be followed, but by ensuring that harm is minimized. They choose to visit medical professions for khatna. For others, the risks of khatna outweigh its religious importance, and they have decided to abandon the practice. For others, consent is crucial, and believe khatna requires a girl’s consent. Since children are incapable of giving informed consent, people believe their daughters can choose to undergo the procedure as an adult, thereby making an informed decision. Thus, the religious clergy’s pastoral power plays an important role in influencing people’s decision to continue khatna. Medicalisation of FGM/C can help negotiate embracing tradition and modernity. However, law also plays an important role in helping end the practice. The growing discourse around the practice has led to people making informed, conscious decisions about following khatna. FGM/C is conceptualized as a health and human rights issue, and a children’s rights issue, which is universal. Thus, efforts against FGM/C should be focused on balancing universalization of children’s rights, human rights, and multiculturalism. Additionally, law plays a crucial role, because legislation can provide a universal stance against the practice, which can be used as a strong justification against it. Thus, community-wide change is required for individual families to abandon FGM/C, through education and activism from within the community, backed by law.
Here’s what a new study says about female genital cutting in Malaysia

By Zahra Qaiyumi Female genital cutting (FGC) is prevalent among Muslim women in rural Malaysia, and many of them believe the practice is a religious obligation. Ironically, several religious leaders in the country insist that female genital cutting is not an Islamic requirement at all. These are some of the major findings of a new research study on FGC in Malaysia, conducted by Abdul Rashid and Yufu Iguchi in 2018. The study was conducted in two rural majority Muslim areas of Kedah and Penang in the Northern region of Peninsular Malaysia. The study consisted of survey data collected from 605 participants, focus groups held with a smaller subset of the participants, and interviews with 8 traditional practitioners who perform or performed FGC. Additionally, 2 interviews were conducted with Muftis, who are religious scholars or jurists qualified to issue Islamic legal opinions in Malaysia. The major findings of the study are below. Prevalence and type of FGC: Almost all participants (99.3%) had undergone FGC at an early age and wanted FGC to continue. The predominant form of FGC practiced in Malaysia is type IV. The paper defines this as the tip of the clitoris being nicked using a pen-knife or razor. Age at which FGC was conducted: The median age of the participants at the time of FGC was 6 years old, which is also the median age the participants felt was the suitable age FGC should be performed. However, the authors suggest that children as young as 2 months old undergo FGC in Malaysia. Medicalization of the practice: In general, older participants had FGC performed on them by traditional practitioners as compared with younger participants. Younger participants were of the opinion that doctors should conduct FGC as compared with older participants who preferred traditional practitioners. More participants from the younger group would permit doctors to perform FGC on their children as compared with the older group. More of the practice is being conducted in clinics by physicians because of the scarcity of traditional practitioners. Reasons for the practice and its continuation: The most common reasons for FGC among the participants surveyed are hygiene (25.0%), health (24.0%) and religious obligation (23.0%). A majority of the participants believe FGC is a requirement in religion (wajib), whereas the traditional practitioners and Mufti’s who are responsible for issuing edicts related to religious matters say it is not a religious requirement. Future directions: It is encouraging that traditional practitioners and Mufti’s believe FGC is not a religious requirement. Perhaps this can be used as a tool to better educate the community about the practice of FGC and ultimately bring an end to the practice. Read the complete study on FGC in Malaysia here.
The Disturbing Trend of Medicalising Female Genital Mutilation
by Lorraine Koonce-Farahmand In the Zero Tolerance campaign to end Female Genital Mutilation (FGM), what has been noted is the arc of progress. Increasingly, women and men from practising groups have declared support for ending FGM; and in several countries, the prevalence of FGM has decreased significantly. A BMJ Global Health study reported that the rates of FGM have fallen dramatically amongst girls in Africa in the last two decades. Using data from 29 countries going back to 1990, the BMJ study found that the biggest fall in cutting was in East Africa where the prevalence rate dropped from 71% of girls under 14 in 1995, to 8% in 2016. Some countries with lower rates – including Kenya and Tanzania, where 3-10% of girls endure FGM – helped drive down the overall figure. Nevertheless, UNICEF’s groundbreaking report shows that whilst much progress has been made in abandoning FGM, millions of girls are still at risk. Flourishing against this backdrop is the compromise of medicalisation of FGM that competes against progress in the Zero Tolerance Campaign. A disturbing number of parents are seeking out healthcare providers to perform FGM. According to the World Health Organization (WHO), medicalisation is when a healthcare provider performs FGM in a clinic or elsewhere. Such procedures are usually paid for under the assumption that medicalisation is not FGM, and is done to mitigate health risks associated with the practice. Consequently, in recent years, the medicalisation of FGM has taken place globally, particularly in Egypt, Indonesia, Kenya, Malaysia, Mali, Nigeria, Northern Sudan, and Yemen. In many of these countries, one-third or more of women had their daughters cut by medical staff with access to sterile tools, anesthetics, and antibiotics. The non-governmental organization, 28 Too Many has investigated the involvement of health professionals and has highlighted what must be done to reverse this trend. 28 Too Many reported that the medicalisation of FGM in Egypt is an enormous challenge. Currently, 78.4% of incidences of FGM in Egypt are carried out by health professionals. Egypt had the highest rate of health workers performing FGM at 75%, with Sudan at 50% and Kenya at 40%. A 2016 study by The United Nations International Children’s Emergency Fund (UNICEF) and the Africa Coordinating Centre for the Abandonment of FGM/C (ACCAF) also found that FGM is increasingly being performed by medical practitioners. Parents and relatives seek safer procedures, rather than outright abandon FGM. The medicalisation trend has conveniently forgotten that FGM violates women’s and children’s human rights to health, to be free from violence, to have the right to physical integrity and non-discrimination, and to be free from cruel, inhumane, and degrading treatment. The “just a nick” is essentially gender-based violence (GBV). What is being “nicked” is still part of a woman’s labia majora, labia minora or clitoris. The medicalisation of FGM perpetuates that women are inferior human beings. This is not in harmony with international human rights standards. There is also clearly an economic incentive for promoting medicalisation. Medical personal perform it for financial gain under the premise that if the crux of the issue is the health side effects and pain, by using sterilised instruments and medication the problem has dissipated. The misguided assertion that medicalisation is a viable option is ignoring the fact that all types of FGM have been recognised as violating human rights. These rights that have been codified in several international and regional treaties mirror worldwide acceptance and political consensus at various UN world conferences and summits. Committees such as The Committee on the Elimination of All Forms of Discrimination against Women, (CEDAW), the Committee on the Rights of the Child, and The Human Rights Committee have been active in condemning FGM. Medicalisation goes against the principles enshrined in these treaties and conventions. The disturbing medicalization trend continues to argue that this less severe form of FGM can protect girls and women from harm. This was echoed in The Economist article of June 18th, 2016, ‘Female Genital Mutilation: an Agonising Choice’Female Genital Mutilation: an Agonising Choice’. In the article, it was asserted that because three decades of campaigning for a total ban on FGM have failed, a new approach is warranted. The article advocated “nicking” of girl’s genitals by trained health professionals as a lesser evil. This reasoning was echoed in the Journal of Medical Ethics by two U.S.-based doctors, Dr. Kavita Shah Arora, Director of Quality, Obstetrics, and Gynaecology at the MetroHealth Medical Center in Cleveland, and Dr. Allan Jacobs, Professor of Reproductive Medicine at Stony Brook University. They wrote that “we must adopt a more nuanced position that acknowledges a wide spectrum of procedures that alter female genitalia.” They assert that they do not believe minor alterations of the female genitalia reach the threshold of a human rights violation. They also asserted that the nicking of the vulva and removing the clitoral hood should not be considered child abuse. They posit that by undergoing these acceptable procedures in the U.S. during infancy, girls can avoid the risk of being sent abroad for more extensive procedures. These doctors and writers from influential respected journals are often held in high esteem by decision-makers, policy-makers, and experts. However, the advocation of medicalisation grotesquely undermines the hard and courageous work undertaken to end FGM worldwide. The medicalisation trend has ostensibly failed to recognise that the proposal of removing the clitoral hood and “just nicking” the vulva contradicts the WHO’s statement that there is absolutely no reason, medical, moral or aesthetic, to cut any part of these exterior organs. There are compelling reasons why the medicalisation of FGM is fundamentally wrong. The medicalisation is and would be carried out on young girls between infancy and the age of 15. Medicalisation is an attack against the sexual and psychological integrity of young girls. Many are not in a position to say no, unable to give informed consent or to effectively resist the practice. Medicalisation reflects a deep-rooted inequality between the sexes and constitutes an extreme form of discrimination against women.
How doctors responded to my genital mutilation: An American woman’s 70-year journey

By A. Renee Bergstrom, EdD Country of Residence: United States Renee chronicles her experiences with American physicians from the time she was cut at three years of age until seventy years later when she became an advocate against female genital mutilation. She also shared her story during the Sahiyo Stories Workshop to encourage other women to speak out. 1947—age 3—My mother took me to a doctor because she was concerned that my little face turned red when I touched my clitoris. This fundamentalist Christian physician believed masturbation to be a sin and practiced his religion with a scalpel in a Wahpeton, North Dakota, clinic. He removed my visible clitoris. Some of my sensitive tissue fused to my inner labia. 1959—age 15—I drove myself to the same clinic not realizing this was where my mutilation took place. I complained to the doctor about the uncomfortable tugging sensation from my scar. He did not examine me or offer a solution. (Separating the scar may have solved the problem.) Instead, he gave me a brochure on the sin of self-pleasuring. 1965—age 21—During my premarital examination (why were these required?), I told the doctor I was not sure I would be able to have “normal” orgasms like other women. He faced the wall and did not comment. 1967—age 23—During my first childbirth, my scar did not stretch, so second stage labor came to a halt. I was given anesthesia against my will and did not wake up until four hours after our daughter was born. My obstetrician had performed an extensive episiotomy to enable her to be delivered vaginally. He did not mention the details of my birthing experience while I was in the hospital or at my six-week postpartum checkup. Later, when intercourse was uncomfortable and my vagina seemed lumpy, I returned to discuss the problem. He showed me pictures of normal female genitalia in an anatomy book and said, “Renee, you don’t look like other women.” He thought I could have had a bike accident as a child. He was shocked when I told him my story. I believe he prescribed lubricating gel to use until I healed completely, which took a couple of months. 1968—age 24—When I was pregnant with our second child, I made an appointment with the same obstetrician. I waited and waited in the examination room and finally another obstetric physician came in. He said the other doctor was leaving to put IUDs in African women and would not be available to provide my care. In retrospect, I think his experience with me touched him deeply and he couldn’t face me to say goodbye. I came home crying and my husband thought there was something wrong with the baby. I had hoped to continue my obstetrical care with this compassionate physician so I felt a great loss. The next doctor assigned to me urged me to allow him to connect me with William Masters and Virginia Johnson of the research team. He thought they would be interested in my sexual response and would pay me well to participate in experiments. He suggested this at every visit and I repeatedly declined. He anesthetized me for the delivery. I awakened in a cold delivery room with my feet still in the stirrups, my episiotomy unstitched and my struggling son in a bassinet out of my reach. The OB team had left me to attend to another woman’s emergency. 1970—age 25—I gave birth to our second son eleven months after his brother was born. I was semi-awake as he moved through the birth canal. The baby urinated immediately and the doctor held him so he peed in my face. I missed the first two birthing experiences and this rude, unfeeling man tainted the one when I was alert. Being cut took away my dream of the deeply spiritual joy of birthing. 1981—age 37—I began my End FGM advocacy when I received funding from the Women’s Desk of the Lutheran World Federation to spend two weeks in Geneva, Switzerland, discussing the issue with international organizations there. My empathetic primary care physician was required to write a letter confirming that I was indeed cut. 1981—In preparation for my 1981 Geneva trip, I attended the University of Minnesota Week of Enrichment designed to help doctors, pastors and therapists respond compassionately to those who bring a variety of sexual issues to them. This allowed me to practice telling my story in a small group supportive environment. When word got out that I was in attendance, a surgeon came and offered to create a faux clitoris for me with one of my nipples. I thought about it for awhile, then declined the offer in the parking lot while she stood next to her car. She was visibly angry, so I responded, “Why should I allow another part of my body to be mutilated when sexual intercourse is sufficiently satisfying?” Later 1980s—age 40s—Two physician interactions stand out in my memory. I saw a dermatologist for a boil on my labia. When I shared my genital history, she was furious. Such a refreshing response! Previous physicians hid their emotions as if to protect the medical profession. The second experience was disturbing. I fell on metal bleachers at our children’s track meet with a resulting large hematoma on my labia. The beautiful young emergency room physician appeared to suggest that my husband had caused the injury, probably because she saw my strangely mutilated body. I didn’t provide details because there were thin curtains separating me from other patients. A couple of weeks later, we read that she walked into a lake and ended her life. I wonder if she just couldn’t tolerate witnessing the abuse cases she faced in the E.R. 1997—age 53—My genital scar began to separate. My very caring female primary care physician helped me deal with the pain and taught me to massage the area to speed the process, finally ending fifty years of the annoying tugging sensation. 2017—age 73—After several years of sharing my
